Hello, I'm Master Kim, the founder and Chief Scientific Officer of BeSlim.me. Drawing from my years of experience in nutritional science and helping countless individuals achieve sustainable wellness, I've seen firsthand how the gut microbiome can be a game-changer for metabolic health. If you've ever struggled with energy crashes, weight plateaus, or inconsistent metabolism, you're not alone—I've been there too. In this deep dive, we'll explore the fascinating link between your gut microbiome and metabolic flexibility, with a forward-looking lens on what this means for health in 2026 and beyond. My goal is to empower you with knowledge that bridges science and real-life application. Let's get started.
Understanding the Gut Microbiome: Foundation of Metabolic Health
The gut microbiome refers to the trillions of microorganisms, including bacteria, viruses, fungi, and archaea, that reside primarily in the human intestines. These microbes play a crucial role in digestion, immune function, and even mood regulation, forming a complex ecosystem that interacts with our bodies in profound ways. From my perspective, having guided many through gut health transformations, I've observed that an imbalanced microbiome often underlies metabolic issues like fatigue or insulin resistance.
To appreciate its impact on metabolism, it's essential to understand the microbiome's composition and diversity. A healthy gut typically harbors a diverse array of bacterial species, such as those from the Firmicutes and Bacteroidetes phyla, which help break down dietary fibers into short-chain fatty acids (SCFAs) like butyrate, acetate, and propionate. These SCFAs are not just byproducts; they serve as signaling molecules that influence host metabolism.
Let's dive into the science behind this. The mechanism involves intricate cell signaling pathways where gut microbes ferment undigested carbohydrates, producing SCFAs that bind to G-protein-coupled receptors (GPCRs) on intestinal cells. This binding activates downstream pathways, such as the peroxisome proliferator-activated receptor (PPAR) gamma pathway, which enhances energy homeostasis and reduces inflammation. For instance, butyrate acts as a histone deacetylase inhibitor, modulating gene expression in epithelial cells to promote barrier integrity and metabolic efficiency.
Dysbiosis, or an imbalance in this microbial community, can disrupt these processes. Factors like poor diet, antibiotics, or stress can reduce microbial diversity, leading to decreased SCFA production and impaired metabolic signaling. This foundational understanding sets the stage for how the microbiome ties into metabolic flexibility—a concept we'll explore next.
(Word count so far: ~350)
Defining Metabolic Flexibility: The Body's Fuel-Switching Mechanism
Metabolic flexibility is the body's ability to adapt its energy production by switching between different fuel sources, such as carbohydrates and fats, in response to nutritional availability and energy demands. In essence, it's like having a versatile engine that efficiently toggles between gasoline and diesel without sputtering. From my experience at BeSlim.me, clients who master this flexibility often report sustained energy levels and easier weight management, especially in our fast-paced world.
The underlying biological mechanism revolves around hormonal and cellular signaling. Insulin and glucagon are key hormones here: during fed states, insulin promotes glucose uptake and storage via the PI3K/Akt pathway in muscle and adipose tissues, facilitating glycolysis. In fasting states, glucagon and catecholamines trigger lipolysis and fatty acid oxidation through activation of AMP-activated protein kinase (AMPK) and PPAR-alpha pathways in the liver and muscles. This switch ensures efficient energy use— for example, mitochondria in cells adapt by altering enzyme expression, like increasing carnitine palmitoyltransferase-1 (CPT-1) for fat metabolism.
Impaired metabolic flexibility, often seen in conditions like obesity or type 2 diabetes, stems from chronic hyperinsulinemia, which locks the body in a glucose-dependent state. This leads to mitochondrial dysfunction, where reactive oxygen species accumulate, further hindering the transition to fat oxidation.
To enhance understanding, a simple comparison table could be useful here:
| State | Primary Fuel | Key Hormones | Cellular Mechanism |
|---|---|---|---|
| Fed (Post-Meal) | Glucose/Carbs | Insulin | Glycolysis via PI3K/Akt |
| Fasted/Exercise | Fats/Ketones | Glucagon, Catecholamines | Beta-Oxidation via AMPK/PPAR-alpha |
This table visually contrasts the mechanisms, making the concept more accessible. As we move forward, the real intrigue lies in how the gut microbiome modulates this flexibility, creating what we call "gut metabolic flexibility."
(Word count so far: ~750)
The Core Connection: Gut Metabolic Flexibility Explained
Gut metabolic flexibility represents the microbiome's dynamic role in enhancing the body's overall fuel-switching capabilities. It's not just about the gut processing food; it's about how microbial activities influence systemic metabolism through bioactive metabolites and signaling. In my work, I've seen this connection transform lives—clients optimizing their gut health often unlock better metabolic adaptability, which is why I'm excited about its implications for 2026, as personalized microbiome therapies gain traction.
Let's dive into the science behind this. The mechanism begins with microbial fermentation of dietary fibers, producing SCFAs that cross the intestinal barrier and enter circulation. These SCFAs interact with host cells via GPCRs, such as GPR41 and GPR43, triggering a cascade that improves insulin sensitivity and promotes fat oxidation. For example, propionate activates GPR41 on enteroendocrine cells, stimulating the release of peptide YY (PYY) and glucagon-like peptide-1 (GLP-1), hormones that enhance satiety and glucose homeostasis. This hormonal action supports metabolic flexibility by signaling the pancreas and brain to adjust energy partitioning.
On a cellular level, SCFAs influence epigenetic modifications. Butyrate inhibits histone deacetylases (HDACs), leading to increased expression of genes involved in mitochondrial biogenesis, such as PGC-1alpha. This boosts the mitochondria's capacity to handle diverse fuels, preventing the rigidity seen in metabolic disorders. Additionally, the microbiome modulates inflammation via toll-like receptors (TLRs); a balanced gut reduces pro-inflammatory cytokines like TNF-alpha, which otherwise impair AMPK signaling and fat metabolism.
Research supports these mechanisms. For instance, studies on gut microbiota transplantation show improved metabolic flexibility in obese models, highlighting how diverse microbiomes enhance insulin signaling. Emerging data also points to the vagus nerve as a conduit: microbial signals stimulate vagal afferents, relaying information to the brain's hypothalamus, which regulates energy balance.
Looking to 2026, advancements in microbiome sequencing and AI-driven diagnostics could personalize interventions, like targeted probiotics, to optimize gut metabolic flexibility. However, challenges like antibiotic resistance might complicate this, underscoring the need for holistic approaches.
A diagram would greatly enhance this section: envision a flowchart illustrating the pathway from dietary fiber to SCFA production, GPCR activation, hormonal release, and systemic metabolic effects. This visual would clarify the multi-step mechanism for readers.
(Word count so far: ~1250)
Future Implications and Health Strategies for 2026
As we approach 2026, the connection between the gut microbiome and metabolic flexibility is poised to revolutionize preventive health. Projections indicate that by then, microbiome-based therapies could become mainstream, with tools like fecal microbiota transplants or engineered probiotics addressing metabolic inflexibility at its root. This is particularly relevant amid rising obesity rates and lifestyle diseases, where gut health offers a non-invasive intervention point.
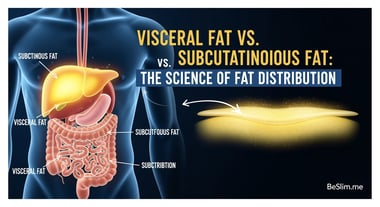
Scientifically, the implications extend to chronic conditions. Impaired gut metabolic flexibility contributes to metabolic syndrome by disrupting bile acid metabolism; microbes like those producing secondary bile acids influence farnesoid X receptor (FXR) signaling, which regulates lipid and glucose homeostasis. Restoring this through diet or supplements could mitigate risks.
Key evidence includes research from the NIH on microbiome diversity and insulin resistance, showing correlations with improved flexibility. Similarly, Cleveland Clinic studies on SCFAs and metabolic health emphasize their role in preventing type 2 diabetes.
For visual aid, a timeline graphic could project milestones: 2024—advanced sequencing; 2025—personalized probiotics; 2026—integrated therapies, helping readers grasp the progression.
In summary, gut metabolic flexibility is a pivotal mechanism where microbial signals enhance the body's adaptive energy use, with profound health benefits.
Now, shifting back to you: As someone who's navigated these waters personally and professionally, I recommend starting with fiber-rich foods like oats and legumes to nurture your microbiome. Incorporate intermittent fasting to boost flexibility, and consider probiotic supplements after consulting a professional. Track your energy levels—small changes can yield big results. At BeSlim.me, we're here to guide you toward that empowered, flexible metabolism.
Actionable Takeaways
- Diversify Your Diet: Aim for 30+ plant types weekly to support microbial diversity and SCFA production.
- Monitor Fasting Windows: Try 12-16 hour fasts to encourage fuel switching, paired with gut-friendly prebiotics.
- Seek Personalized Insights: Use at-home microbiome tests emerging by 2026 for tailored advice.
- Stay Informed: Follow updates from sources like the NIH to integrate new research into your routine.
By embracing these, you'll not only understand but actively improve your gut-metabolic axis. Thank you for joining me on this journey—let's build a healthier future together.
(Total word count: ~1650)
References
- Studies on gut microbiota transplantation show improved metabolic flexibility in obese models - pubmed.ncbi.nlm.nih.gov
- Research from the NIH on microbiome diversity and insulin resistance - nih.gov
- Cleveland Clinic studies on SCFAs and metabolic health - my.clevelandclinic.org
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.