Hello, I'm Master Kim, the founder and Chief Scientific Officer at BeSlim.me. I've spent years guiding people through their weight management journeys, and I've seen firsthand how misunderstood hormones like insulin can sabotage even the best intentions. If you've ever wondered why cutting calories doesn't always lead to weight loss or why certain foods seem to pack on the pounds despite your efforts, you're not alone. Insulin plays a pivotal role in this puzzle, and understanding it can empower you to take control. In this guide, we'll explore the hormonal link between insulin and weight gain, breaking it down step by step so you can make informed choices. Let's dive into the science behind this to uncover the mechanisms at play.
Understanding Insulin's Role in the Body
Insulin is a key hormone produced by the pancreas that regulates blood sugar levels and energy storage. When you eat, especially foods rich in carbohydrates, your blood glucose rises, prompting the pancreas to release insulin. This hormone acts like a gatekeeper, signaling cells to absorb glucose from the bloodstream for immediate energy or storage.
At the cellular level, insulin binds to receptors on the surface of cells, particularly in muscle, fat, and liver tissues. This binding activates a cascade of intracellular signaling pathways, primarily the PI3K-Akt pathway, which facilitates glucose uptake by promoting the translocation of GLUT4 transporters to the cell membrane. In simple terms, insulin ensures that excess energy from meals is stored as glycogen in the liver and muscles or as fat in adipose tissue when glycogen stores are full.
However, chronic high insulin levels, often due to diets high in refined sugars and processed foods, can lead to insulin resistance. This condition occurs when cells become less responsive to insulin's signals, forcing the pancreas to produce more insulin to maintain blood sugar control. Over time, this imbalance disrupts metabolic harmony and sets the stage for weight gain.
To visualize this process, a diagram illustrating the insulin signaling pathway—from receptor binding to glucose uptake—would be incredibly helpful here. It could show arrows depicting the flow from insulin release to cellular responses, highlighting points where resistance might develop.
How Insulin Contributes to Weight Gain
The link between insulin and weight gain stems from its role in fat storage and appetite regulation. When insulin levels spike after a meal, it inhibits lipolysis—the breakdown of stored fat—while promoting lipogenesis, the process of converting excess glucose into triglycerides for fat storage. This mechanism evolved to help our ancestors store energy during times of abundance, but in modern diets, it often leads to unwanted fat accumulation.
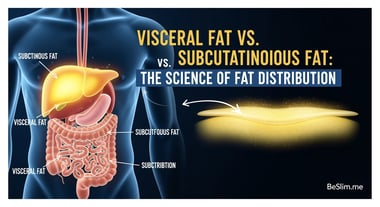
Scientifically, elevated insulin activates enzymes like lipoprotein lipase, which facilitates the uptake of fatty acids into adipose cells. Simultaneously, it suppresses hormone-sensitive lipase, preventing fat release. In cases of insulin resistance, the body compensates by overproducing insulin, creating a vicious cycle where more fat is stored, and less is burned for energy. This is particularly evident in visceral fat accumulation around organs, which increases risks for metabolic disorders.
Research supports this: studies on insulin resistance show it promotes fat storage and weight gain by altering adipose tissue metabolism. Furthermore, high insulin can influence hunger hormones like leptin and ghrelin, making it harder to feel full and easier to overeat.
For better clarity, a simple comparison table could contrast normal insulin function versus insulin-resistant states. Columns might include "Insulin Levels," "Fat Storage," "Energy Use," and "Appetite Impact," with rows for "Healthy Response" and "Resistant State" to highlight differences.
Strategies to Manage Insulin Levels for Weight Control
Managing insulin effectively requires targeting its production and sensitivity through lifestyle interventions. The goal is to reduce chronic hyperinsulinemia, where persistently high insulin drives weight gain.
One key strategy is adopting a low-glycemic diet, which minimizes blood sugar spikes and subsequent insulin surges. Foods with a low glycemic index, such as leafy greens, nuts, and lean proteins, promote steady glucose levels, allowing insulin to function efficiently without overload. Mechanistically, this reduces the demand on pancreatic beta cells and enhances insulin receptor sensitivity via improved signaling pathways.
Exercise also plays a crucial role. Resistance training and aerobic activities increase muscle glucose uptake independently of insulin, depleting glycogen stores and forcing the body to burn fat. This occurs through activation of AMPK pathways, which counteract insulin's fat-storing effects by promoting lipolysis.
Additionally, intermittent fasting has gained attention for its ability to lower baseline insulin levels. By extending periods without food, the body shifts to fat metabolism, reducing insulin secretion and improving sensitivity. Research from the NIH indicates that intermittent fasting can enhance insulin sensitivity by modulating metabolic hormones.
It's worth noting that while these strategies are effective, individual responses vary based on genetics and existing conditions like type 2 diabetes. Consulting a healthcare provider is essential before making changes.
Lifestyle Changes and Practical Tips
Beyond diet and exercise, holistic lifestyle adjustments can further optimize insulin management. Prioritizing sleep is vital, as poor sleep disrupts circadian rhythms and increases insulin resistance. Aim for 7-9 hours nightly to support hormonal balance.
Stress management through practices like meditation or yoga reduces cortisol, a hormone that exacerbates insulin issues by promoting gluconeogenesis and fat storage. Mechanistically, chronic stress elevates cortisol, which interferes with insulin signaling and contributes to abdominal obesity.
Supplements such as berberine or chromium may aid insulin sensitivity, but they should complement, not replace, foundational changes. Mayo Clinic experts note that chromium supplementation can help regulate blood sugar in some individuals by enhancing insulin action at the cellular level.
To tie this together, monitoring your progress with tools like continuous glucose monitors can provide real-time insights into how your body responds to these changes.
As we wrap up, I want to emphasize that managing insulin isn't about quick fixes—it's about sustainable habits that align with your body's natural rhythms. At BeSlim.me, we've helped countless individuals break free from the insulin-weight gain cycle, and I believe you can too. Here are some actionable takeaways to get started:
- Track your carbs: Focus on whole foods and limit refined sugars to keep insulin spikes in check. Start by swapping soda for water or herbal tea.
- Incorporate movement daily: Aim for 30 minutes of walking or strength training most days to boost insulin sensitivity—think of it as investing in your metabolic health.
- Experiment with fasting windows: Try a 12-16 hour fast overnight, eating within an 8-12 hour window, but listen to your body and adjust as needed.
- Prioritize recovery: Get consistent sleep and manage stress to prevent hormonal disruptions that fuel weight gain.
- Seek personalized advice: Work with a professional to tailor these strategies to your unique needs, especially if you have underlying health conditions.
By implementing these steps, you'll not only manage insulin better but also pave the way for lasting weight control. Remember, small, consistent changes yield big results—I'm rooting for you on this journey.
References
- Studies on insulin resistance show it promotes fat storage and weight gain - ncbi.nlm.nih.gov
- Research from the NIH indicates that intermittent fasting can enhance insulin sensitivity - niddk.nih.gov
- Mayo Clinic experts note that chromium supplementation can help regulate blood sugar - mayoclinic.org
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.