Hello, I'm Master Kim, the founder and Chief Scientific Officer at BeSlim.me. Over the years, I've worked with countless individuals struggling with persistent hunger and weight management challenges. I know how frustrating it can be when you feel like you're always fighting an uphill battle against your own appetite. That's why I'm passionate about breaking down complex topics like leptin resistance—it's often the hidden culprit behind that constant hunger. In this article, we'll explore what leptin resistance really means, why it happens, and how understanding it can empower you to take control. Let's dive into the science behind this.
Understanding Leptin: The Body's Hunger Regulator
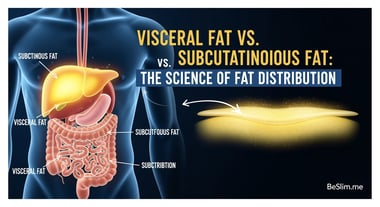
Leptin is a hormone primarily produced by fat cells, or adipocytes, in the body. Its main function is to signal to the brain when you've had enough to eat, helping regulate energy balance and body weight. When fat cells release leptin into the bloodstream, it travels to the hypothalamus—a key region in the brain responsible for controlling hunger and metabolism.
The process begins at the cellular level. Leptin binds to specific receptors on neurons in the hypothalamus, activating a signaling pathway that suppresses appetite and increases energy expenditure. This mechanism ensures that as your body fat increases, more leptin is produced, which should naturally reduce your food intake and prevent excessive weight gain. Conversely, when fat stores are low, leptin levels drop, signaling the body to eat more and conserve energy.
To visualize this, imagine leptin as a messenger carrying a "stop eating" note from your fat tissues to your brain. When everything works smoothly, this communication keeps your hunger in check. However, disruptions in this pathway can lead to issues like constant hunger.
Let's dive into the science behind this. Research shows that leptin plays a crucial role in long-term energy homeostasis. For instance, in healthy individuals, leptin signaling effectively reduces food intake by modulating neuropeptide Y and pro-opiomelanocortin neurons in the hypothalamus, which are key players in appetite regulation.
This foundational understanding sets the stage for why leptin resistance disrupts this balance. A simple comparison table here could enhance clarity: one column for "Normal Leptin Function" (e.g., high leptin leads to reduced hunger) versus "Disrupted Function" (e.g., high leptin but no appetite suppression), highlighting the differences in outcomes.
What Causes Leptin Resistance?
Leptin resistance occurs when the brain no longer responds adequately to leptin signals, even though leptin levels in the blood may be high. This condition is akin to insulin resistance in diabetes, where the body produces the hormone but cells fail to respond properly. As a result, the hypothalamus doesn't receive the "full" signal, leading to persistent hunger, overeating, and difficulty losing weight.
Several factors contribute to the development of leptin resistance. Chronic inflammation, often linked to obesity, can interfere with leptin receptor sensitivity. High levels of triglycerides in the blood may also block leptin's transport across the blood-brain barrier, preventing it from reaching the hypothalamus effectively.
From a biological perspective, leptin resistance involves impaired cell signaling. Normally, leptin activates the JAK-STAT pathway within hypothalamic neurons, which inhibits hunger-promoting neurons and activates those that promote satiety. In resistance states, this pathway becomes desensitized, often due to overactivation or inflammatory cytokines disrupting receptor function.
The mechanism is further complicated by feedback loops. For example, prolonged high-fat diets can elevate free fatty acids, which impair leptin transport and signaling. This creates a vicious cycle: obesity increases leptin production, but resistance prevents its effects, leading to more fat accumulation.
To illustrate this cycle, a diagram showing the leptin signaling pathway—depicting normal binding versus resistant states with blocked receptors—would be particularly helpful. It could include arrows for hormone release, receptor interaction, and downstream effects on appetite.
Scientific evidence supports these mechanisms. Studies indicate that [obesity-induced inflammation contributes to leptin resistance by altering hypothalamic signaling pathways], emphasizing the role of pro-inflammatory molecules like TNF-alpha in desensitizing leptin receptors.
The Biological Mechanisms of Leptin Resistance in Detail
Delving deeper into the cellular level, leptin resistance involves intricate disruptions in hormone action and cell signaling. Leptin binds to its receptor (LEPR), a member of the cytokine receptor family, triggering phosphorylation of Janus kinase 2 (JAK2). This activates signal transducer and activator of transcription 3 (STAT3), which translocates to the nucleus and regulates gene expression for appetite control.
In leptin-resistant states, several mechanisms impair this process. One key issue is suppressor of cytokine signaling 3 (SOCS3) overexpression, which inhibits JAK-STAT signaling by binding to phosphorylated JAK2, effectively turning off the pathway. Chronic hyperleptinemia—persistently high leptin levels—upregulates SOCS3, creating resistance.
Another mechanism involves endoplasmic reticulum (ER) stress in hypothalamic neurons. Obesity and high-fat intake induce ER stress, leading to unfolded protein response that disrupts leptin signaling. Additionally, impaired blood-brain barrier transport due to elevated triglycerides prevents leptin from accessing its target neurons.
At the molecular level, alterations in AMP-activated protein kinase (AMPK) and phosphatidylinositol 3-kinase (PI3K) pathways contribute. Normally, leptin activates AMPK to increase energy expenditure, but in resistance, this activation fails, reducing metabolic rate and perpetuating hunger.
These mechanisms explain why individuals with leptin resistance often feel "always hungry" despite adequate or excess body fat. The brain perceives a state of starvation, driving compulsive eating behaviors.
For better understanding, a comparison table could contrast "Healthy Leptin Signaling" (e.g., efficient JAK-STAT activation, reduced hunger) with "Leptin-Resistant Signaling" (e.g., SOCS3 inhibition, persistent hunger), including key molecules involved.
Supporting this, research from authoritative sources highlights that endoplasmic reticulum stress in the hypothalamus is a critical factor in obesity-related leptin resistance, linking it to global obesity trends and hormonal dysregulation.
Managing Leptin Resistance: Strategies and Actionable Takeaways
Leptin resistance isn't irreversible, and addressing it through lifestyle changes can restore sensitivity and curb constant hunger. The focus is on reducing inflammation, improving diet quality, and enhancing overall metabolic health.
From a scientific standpoint, interventions like caloric restriction and exercise have shown promise in reversing resistance by lowering leptin levels and improving receptor sensitivity. Anti-inflammatory diets rich in omega-3 fatty acids can mitigate cytokine interference with signaling pathways.
Now, shifting back to you—I've seen these strategies work wonders for many at BeSlim.me. Here are some actionable takeaways to get started:
Adopt an Anti-Inflammatory Diet: Prioritize whole foods like fatty fish, nuts, and vegetables to reduce inflammation. Avoid processed sugars and trans fats that exacerbate resistance.
Incorporate Regular Exercise: Aim for 150 minutes of moderate activity per week, such as walking or strength training, to enhance leptin sensitivity and boost metabolism.
Prioritize Sleep and Stress Management: Get 7-9 hours of quality sleep nightly and practice mindfulness to lower cortisol, which can worsen resistance.
Monitor Progress Mindfully: Track your hunger levels and energy in a journal; consult a healthcare provider for personalized advice, especially if you suspect underlying conditions.
By implementing these steps, you can break the cycle of constant hunger and move toward sustainable weight management. Remember, consistency is key—small changes add up over time.
In summary, leptin resistance disrupts the body's natural hunger regulation through impaired signaling and inflammation, but understanding these mechanisms empowers effective management. If you're ready to take the next step, we're here at BeSlim.me to support your journey.
References
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.