Hello, I'm Master Kim, the Founder and Chief Scientific Officer at BeSlim.me. Having dedicated my career to understanding how our bodies manage weight and energy, I've seen firsthand how insulin resistance can quietly sabotage health goals. If you've ever wondered why despite your best efforts, the scale doesn't budge or your energy dips, you're not alone—I've been there too. In this article, we'll explore insulin resistance, its deep ties to blood sugar and weight gain, and what you can do about it. Let's empower you with knowledge to take control.
Understanding Insulin Resistance: The Basics
Insulin resistance is a condition where the body's cells become less responsive to insulin, a hormone produced by the pancreas that regulates blood sugar levels. Normally, insulin acts like a key, unlocking cells to allow glucose (sugar) from the bloodstream to enter and be used for energy. When resistance develops, this process falters, leading to elevated blood sugar and a cascade of metabolic issues.
This isn't just a minor glitch—it's a foundational problem in many chronic conditions, including type 2 diabetes and obesity. Think of it as your body's alarm system going off, signaling that something in your metabolic machinery needs attention. Factors like poor diet, lack of exercise, genetics, and even stress can contribute, but the core issue lies in how cells interact with insulin over time.
To make this clearer, a simple comparison table could enhance understanding:
| Aspect | Normal Insulin Response | Insulin-Resistant State |
|---|---|---|
| Blood Sugar Control | Efficient glucose uptake into cells | Reduced uptake, leading to high blood sugar |
| Energy Levels | Steady and sustained | Fluctuations, often with fatigue |
| Weight Impact | Balanced fat storage and use | Increased fat accumulation |
This table highlights the stark differences, setting the stage for why insulin resistance often leads to unintended weight gain. As we delve deeper, remember that recognizing these signs early can make all the difference in reclaiming your health.
Let's dive into the science behind this to understand the precise mechanisms at play.
The Biological Mechanisms of Insulin Resistance
Insulin resistance emerges from disruptions in cellular signaling pathways, particularly those involving the insulin receptor and downstream molecules. At the cellular level, insulin binds to receptors on the surface of cells, such as muscle, fat, and liver cells. This binding activates a signaling cascade that includes proteins like IRS-1 (insulin receptor substrate-1) and PI3K (phosphatidylinositol 3-kinase), ultimately leading to the translocation of GLUT4 transporters to the cell membrane. These transporters facilitate glucose entry into the cell, maintaining blood sugar homeostasis.
In insulin-resistant states, chronic exposure to high insulin levels—often from diets rich in refined sugars—desensitizes these receptors. Inflammation plays a key role here, with pro-inflammatory cytokines like TNF-alpha interfering with IRS-1 phosphorylation, blocking the signal. Additionally, excess free fatty acids from adipose tissue can accumulate in non-fat cells, causing lipotoxicity that further impairs insulin signaling. This creates a vicious cycle: the pancreas compensates by producing more insulin (hyperinsulinemia), which exacerbates resistance.
From a hormonal perspective, insulin's action is counterbalanced by hormones like glucagon and cortisol. In resistance, this balance tips, promoting gluconeogenesis (new glucose production) in the liver, even when blood sugar is already high. Mitochondrial dysfunction also contributes, as impaired energy production in cells leads to oxidative stress, further damaging insulin pathways.
A diagram illustrating the insulin signaling pathway would be particularly helpful here, showing the normal cascade versus the blocked points in resistance—for instance, arrows depicting insulin binding, GLUT4 movement, and inflammatory interruptions. This visual could clarify how these molecular events translate to systemic effects.
Research supports these mechanisms; for example, studies on cellular insulin signaling show that chronic inflammation disrupts IRS-1 function, leading to reduced glucose uptake. Understanding these details reveals why insulin resistance isn't just about sugar—it's a profound alteration in how your body processes energy at the molecular level.
How Insulin Resistance Contributes to Weight Gain
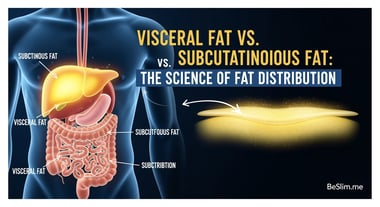
Insulin resistance directly fuels weight gain through altered fat metabolism and energy storage. When cells resist insulin, glucose remains in the bloodstream, prompting the pancreas to release more insulin. This hyperinsulinemia signals the body to store excess energy as fat, particularly in visceral areas around organs, which is metabolically harmful.
Mechanistically, insulin normally inhibits lipolysis (fat breakdown) in adipose tissue while promoting lipogenesis (fat synthesis). In resistance, despite high insulin, fat cells become partially unresponsive, but the liver and muscles' impaired glucose uptake leads to compensatory fat storage elsewhere. Elevated blood sugar also triggers glycation, where sugars bind to proteins, further promoting inflammation and fat accumulation.
Moreover, insulin resistance disrupts appetite regulation via the hypothalamus. Leptin, the satiety hormone from fat cells, signals fullness, but resistance often coincides with leptin resistance, leading to overeating. Ghrelin, the hunger hormone, remains elevated, compounding caloric intake. This hormonal imbalance creates an environment where the body favors fat storage over utilization, even during calorie deficits.
The link to weight gain is evident in metabolic syndrome, where insulin resistance clusters with obesity, high triglycerides, and hypertension. For instance, research from the NIH indicates that insulin resistance promotes visceral fat accumulation, exacerbating weight gain cycles.
To visualize this progression, a flowchart diagram could be useful, mapping how high blood sugar leads to hyperinsulinemia, fat storage, and back to resistance—illustrating the feedback loop that traps many in weight struggles.
These mechanisms explain why traditional dieting often fails without addressing the root insulin issues; it's not just calories in versus out, but how your body handles them.
Strategies to Manage and Reverse Insulin Resistance
Addressing insulin resistance requires targeting its underlying mechanisms through lifestyle interventions that restore cellular sensitivity and hormonal balance. Diet plays a pivotal role: reducing refined carbohydrates lowers blood sugar spikes, allowing insulin levels to normalize and reducing receptor desensitization. Incorporating fiber-rich foods enhances gut health, which influences inflammation via the microbiome-insulin axis.
Physical activity is equally crucial, as exercise activates AMPK (AMP-activated protein kinase), an enzyme that bypasses faulty insulin pathways to improve glucose uptake. Resistance training builds muscle mass, increasing GLUT4 expression independently of insulin, while aerobic exercise reduces visceral fat.
Sleep and stress management are often overlooked but vital; chronic stress elevates cortisol, which antagonizes insulin action, so practices like mindfulness can mitigate this. In advanced cases, medications like metformin work by enhancing insulin sensitivity at the cellular level, but lifestyle remains foundational.
Evidence underscores these approaches: Mayo Clinic guidelines highlight that regular exercise can reverse insulin resistance by improving mitochondrial function, supporting long-term weight management.
By integrating these strategies, individuals can break the cycle of resistance and weight gain, fostering sustainable health.
As we wrap up, I want you to know that overcoming insulin resistance is within reach—I've guided countless people through this at BeSlim.me, and the transformation is real. Here are some actionable takeaways to get started:
- Monitor your carbs: Aim for whole foods over processed ones to stabilize blood sugar—try swapping white rice for quinoa in your meals.
- Move daily: Incorporate 30 minutes of walking or strength training; it directly boosts insulin sensitivity without needing fancy equipment.
- Prioritize sleep: Get 7-9 hours nightly to regulate hormones—create a wind-down routine if needed.
- Track progress: Use a simple blood sugar monitor or consult a doctor for A1C tests to measure improvements.
Remember, small consistent steps lead to big changes. If you're ready to dive deeper, we're here at BeSlim.me to support your journey.
References
- Studies on cellular insulin signaling show that chronic inflammation disrupts IRS-1 function - pubmed.ncbi.nlm.nih.gov
- Research from the NIH indicates that insulin resistance promotes visceral fat accumulation - niddk.nih.gov
- Mayo Clinic guidelines highlight that regular exercise can reverse insulin resistance by improving mitochondrial function - mayoclinic.org
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.