Hello, I'm Master Kim, the founder and Chief Scientific Officer of BeSlim.me. Over the years, I've seen how something as fundamental as the balance in our gut can profoundly impact our overall well-being. If you've ever felt unexplained fatigue, digestive issues, or even mood swings, it might trace back to an imbalance in your gut microbiome—a condition known as gut dysbiosis. I've dedicated my career to exploring these connections, and I'm here to guide you through what this means for your health. Let's explore this together, so you can take informed steps toward better balance.
Understanding the Healthy Gut Microbiome
Before we delve into imbalances, it's essential to grasp what a healthy gut microbiome looks like. The gut microbiome refers to the trillions of microorganisms—bacteria, viruses, fungi, and other microbes—residing primarily in the intestines. These microbes form a complex ecosystem that plays a crucial role in digestion, immune function, and even mental health.
In a balanced state, beneficial bacteria like Bifidobacterium and Lactobacillus dominate, aiding in breaking down food, synthesizing vitamins, and protecting against pathogens. This harmony is maintained through intricate biological mechanisms, such as quorum sensing—a form of cell signaling where bacteria communicate via chemical signals to regulate population density and behavior. For instance, these signals help beneficial microbes outcompete harmful ones by producing antimicrobial compounds.
Hormonal influences also come into play; the gut microbiome interacts with the body's endocrine system, modulating hormones like serotonin, which is largely produced in the gut and affects mood and appetite. A healthy microbiome supports the gut-brain axis, a bidirectional communication pathway involving neural, hormonal, and immunological signaling. This ensures efficient nutrient absorption and a robust barrier against toxins.
To visualize this, a simple comparison table could enhance understanding here:
| Aspect | Healthy Microbiome | Dysbiotic Microbiome |
|---|---|---|
| Bacterial Diversity | High (diverse species) | Low (dominated by few harmful strains) |
| Key Functions | Efficient digestion, strong immunity | Inflammation, poor nutrient absorption |
| Health Impact | Balanced mood and energy | Fatigue, digestive disorders |
This table highlights the stark differences, making the concept more accessible. Now, let's dive into the science behind what happens when this balance is disrupted.
Gut dysbiosis occurs when there's a shift in this microbial community, often leading to a decrease in beneficial bacteria and an overgrowth of pathogenic ones. Research shows that factors like diet, antibiotics, and stress can trigger these changes, altering the microbiome's composition and function gut microbiome diversity and its role in health.
Defining Gut Dysbiosis: The Core Concept
Gut dysbiosis is essentially an imbalance in the gut microbiome, where the normal diversity and function of microbes are disrupted. This isn't just a minor shift; it involves profound changes at the cellular and molecular levels. The core mechanism revolves around altered microbial metabolism and signaling pathways that affect the host's physiology.
Biologically, dysbiosis often stems from dysregulated quorum sensing, where pathogenic bacteria like Clostridium difficile release toxins that inhibit beneficial microbes. This leads to a breakdown in the intestinal barrier, known as increased gut permeability or "leaky gut." Here, tight junction proteins—such as occludin and zonulin—fail to maintain the epithelial lining, allowing harmful substances like lipopolysaccharides (LPS) to enter the bloodstream. LPS, a component of bacterial cell walls, triggers systemic inflammation via Toll-like receptor 4 (TLR4) signaling on immune cells, activating pathways like NF-κB that promote cytokine release.
Hormone action is also implicated; dysbiosis can disrupt the production of short-chain fatty acids (SCFAs) like butyrate, which are metabolites produced by beneficial bacteria through fiber fermentation. Butyrate serves as an energy source for colon cells and regulates histone deacetylase (HDAC) activity, influencing gene expression for anti-inflammatory effects. When SCFAs decline, it hampers this regulation, leading to chronic inflammation.
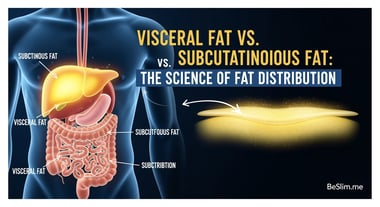
Moreover, the gut-liver axis is affected, where dysbiotic microbes alter bile acid metabolism. Bile acids, synthesized in the liver and modified by gut bacteria, act as signaling molecules via receptors like FXR (farnesoid X receptor), which control lipid and glucose homeostasis. In dysbiosis, abnormal bile acid profiles can exacerbate metabolic disorders.
For better clarity, a diagram illustrating the gut barrier and leaky gut mechanism would be ideal at this point. It could show intact tight junctions in a healthy state versus gaps allowing toxin leakage in dysbiosis, with arrows depicting inflammatory signaling pathways. Such a visual would make these abstract biological processes more tangible.
Studies confirm that dysbiosis is linked to conditions like irritable bowel syndrome (IBS), where microbial shifts correlate with symptom severity gut dysbiosis in irritable bowel syndrome.
How Gut Dysbiosis Impacts Overall Health
The effects of gut dysbiosis extend far beyond the digestive system, influencing multiple organs through interconnected mechanisms. At its core, the imbalance disrupts homeostasis, leading to widespread health issues via inflammatory and metabolic pathways.
One key impact is on the immune system. Dysbiosis impairs the gut's role as an immune training ground, where microbes educate T-cells and regulate immune tolerance. In a dysbiotic state, overactivation of pro-inflammatory Th17 cells occurs, driven by segmented filamentous bacteria, while regulatory T-cells (Tregs) decrease. This imbalance heightens autoimmune responses, as seen in conditions like rheumatoid arthritis, where leaked bacterial products trigger joint inflammation.
Metabolically, dysbiosis affects insulin signaling and glucose metabolism. Reduced SCFA production diminishes activation of G-protein-coupled receptors (GPR41/43) on enteroendocrine cells, which normally release hormones like GLP-1 to enhance insulin sensitivity. Consequently, this can lead to insulin resistance and type 2 diabetes. The gut-brain axis is similarly affected; altered microbial composition reduces serotonin synthesis, impacting neurotransmitter signaling via the vagus nerve and contributing to anxiety or depression.
Cardiovascular health isn't spared either. Dysbiotic microbes promote trimethylamine N-oxide (TMAO) production from dietary choline, which accelerates atherosclerosis by enhancing platelet aggregation and foam cell formation in arteries.
Neurologically, dysbiosis may contribute to neurodegenerative diseases. For example, in Parkinson's disease, alpha-synuclein aggregation might be influenced by gut-derived inflammatory signals crossing the blood-brain barrier.
These mechanisms underscore why addressing dysbiosis is crucial for holistic health. Evidence from clinical reviews supports these links, showing that microbiome alterations are associated with obesity and metabolic syndrome microbiome imbalances in metabolic diseases.
Preventing and Managing Gut Dysbiosis
While dysbiosis can seem daunting, proactive steps can restore balance through targeted interventions that support microbial diversity and function.
Prevention starts with diet: Consuming fiber-rich foods promotes SCFA production, reinforcing the gut barrier. Probiotics and prebiotics can introduce or nourish beneficial bacteria, modulating quorum sensing to favor healthy populations.
Lifestyle factors like stress management are vital, as chronic stress elevates cortisol, which disrupts microbial composition via the hypothalamic-pituitary-adrenal (HPA) axis. Exercise enhances microbial diversity by improving gut motility and reducing inflammation.
For management, fecal microbiota transplantation (FMT) is an emerging therapy that restores balance by transferring healthy microbes, effectively recalibrating signaling pathways. However, it's typically reserved for severe cases like recurrent C. difficile infections.
Monitoring through stool tests can identify imbalances early, allowing personalized interventions. Always consult a healthcare provider before starting supplements or major changes.
To summarize these strategies, a simple flowchart diagram could be suggested here, outlining steps from assessment to intervention, with branches for diet, lifestyle, and medical options. This would provide a practical visual guide.
As we wrap up, remember that small changes can yield big results in restoring your gut health.
Actionable Takeaways
Now that we've explored the science, let's make this personal. I encourage you to start with these steps to support your gut microbiome:
- Incorporate fermented foods: Add yogurt, kimchi, or sauerkraut to your meals 3-4 times a week to boost beneficial bacteria.
- Prioritize fiber: Aim for 25-30 grams daily from sources like oats, beans, and vegetables to fuel SCFA production.
- Manage stress: Practice mindfulness or yoga for 10-15 minutes daily to protect against HPA axis disruptions.
- Seek professional advice: If you suspect dysbiosis, get a microbiome test and discuss probiotics with your doctor.
By taking these actions, you can work toward a healthier, more balanced gut. At BeSlim.me, we're committed to empowering you with science-backed tools for lasting wellness. If you have questions, I'm here to help.
References
- Gut microbiome diversity and its role in health - ncbi.nlm.nih.gov
- Gut dysbiosis in irritable bowel syndrome - mayoclinic.org
- Microbiome imbalances in metabolic diseases - who.int
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.