Hello, I'm Master Kim, the Founder and Chief Scientific Officer at BeSlim.me. Having dedicated years to researching how stress impacts our bodies, I've seen firsthand how chronic tension can lead to stubborn weight gain, especially around the midsection. If you've ever felt like stress is literally weighing you down, you're not alone—I've been there too, and I want to help you understand why this happens and what you can do about it. In this article, we'll explore the science behind the so-called "cortisol belly," breaking it down step by step so you can take informed steps toward better health.
Understanding Cortisol and Its Role in Stress
Cortisol is often called the "stress hormone," and for good reason—it's a key player in how our bodies respond to challenges, both physical and emotional. Produced by the adrenal glands, cortisol helps regulate various functions like metabolism, immune response, and blood pressure. In short bursts, it's beneficial, providing the energy needed to handle acute stressors, such as running from danger or meeting a tight deadline.
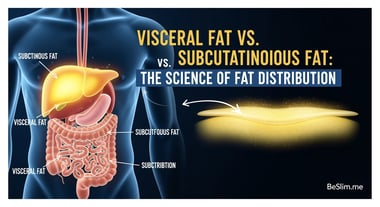
However, when stress becomes chronic—think ongoing work pressure, financial worries, or emotional strain—the body keeps pumping out cortisol at elevated levels. This prolonged exposure can disrupt normal bodily processes, leading to a range of health issues. One of the most visible effects is the accumulation of visceral fat, the deep abdominal fat that wraps around organs like the liver and intestines. Unlike subcutaneous fat (the kind you can pinch under the skin), visceral fat is metabolically active and linked to higher risks of conditions such as insulin resistance and cardiovascular disease.
To visualize this, imagine cortisol as a signal that tells your body to store energy for tough times ahead. In prehistoric days, this might have helped survive famines, but in modern life, it often results in unwanted weight gain, particularly in the belly area. This is where the term "cortisol belly" comes from—a colloquial way to describe the rounded, protruding abdomen that can develop from sustained high cortisol.
Let's dive into the science behind this. Cortisol influences fat distribution through its interaction with other hormones and cellular pathways. For instance, it can increase appetite by stimulating the release of neuropeptide Y, a brain chemical that promotes hunger, especially for high-calorie foods. Over time, this leads to overeating and fat storage, preferentially in the abdominal region due to the higher density of cortisol receptors there.
A simple comparison table could enhance understanding here:
| Aspect | Acute Stress (Short-Term) | Chronic Stress (Long-Term) |
|---|---|---|
| Cortisol Effect | Mobilizes energy for immediate use | Promotes fat storage, especially visceral |
| Health Impact | Temporary boost in alertness | Increased risk of metabolic disorders |
| Fat Distribution | Even or minimal change | Concentrated in abdomen |
This table highlights how the body's response shifts from adaptive to problematic with prolonged stress.
The Biological Mechanism of Cortisol Belly
The mechanism behind cortisol belly involves intricate cell signaling and hormone actions that favor visceral fat accumulation. At the cellular level, cortisol binds to glucocorticoid receptors found in various tissues, including fat cells (adipocytes). In the abdomen, these receptors are more abundant in visceral fat compared to subcutaneous fat, making the belly area particularly susceptible.
When cortisol binds to these receptors, it activates a cascade of events. First, it enhances lipogenesis—the process of converting sugars and other nutrients into fat—while inhibiting lipolysis, the breakdown of fat for energy. This is mediated through enzymes like lipoprotein lipase, which cortisol upregulates in visceral adipose tissue, leading to increased fat uptake from the bloodstream.
Moreover, cortisol disrupts insulin signaling. Normally, insulin helps cells absorb glucose for energy, but high cortisol levels promote insulin resistance, where cells become less responsive. This results in elevated blood sugar, which the body then stores as fat, again favoring the visceral depots. The hypothalamus-pituitary-adrenal (HPA) axis plays a central role here: chronic stress overactivates the HPA axis, leading to sustained cortisol release. This axis involves the brain's hypothalamus releasing corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to secrete adrenocorticotropic hormone (ACTH), ultimately prompting the adrenals to produce cortisol.
On a deeper level, cortisol influences gene expression via the glucocorticoid receptor, which acts as a transcription factor. It can upregulate genes involved in inflammation and fat storage, such as those for cytokines like interleukin-6, contributing to a pro-inflammatory state that exacerbates visceral fat gain. This inflammatory response further perpetuates the cycle, as inflamed fat tissue releases more signals that keep the HPA axis active.
For better clarity, a diagram illustrating the HPA axis and cortisol's pathway to fat cells would be ideal. It could show arrows from the brain to the adrenals, then to abdominal fat, with labels for key hormones and receptors. Such a visual would make the complex signaling more accessible.
Scientific evidence supports these mechanisms. For example, studies on chronic stress show elevated cortisol linked to increased visceral fat, highlighting how prolonged HPA activation correlates with abdominal obesity.
Scientific Evidence and Health Implications
Research consistently links high cortisol levels to visceral fat accumulation, with implications for overall health. Numerous studies have examined populations under chronic stress, such as caregivers or those with high-stress jobs, finding that elevated urinary or salivary cortisol correlates with greater waist circumference and visceral fat mass, as measured by imaging techniques like CT scans.
One key finding is that cortisol promotes the redistribution of fat from peripheral areas (like arms and legs) to the central abdomen. This is partly due to cortisol's catabolic effects on muscle tissue, breaking it down for energy, which indirectly supports fat storage elsewhere. In women, this effect can be amplified during perimenopause, when hormonal shifts make the body more sensitive to stress-induced fat gain.
Health risks associated with cortisol belly are significant. Visceral fat is not just cosmetic; it's endocrinologically active, secreting adipokines that can lead to systemic inflammation and metabolic syndrome. This includes higher chances of type 2 diabetes, hypertension, and heart disease. For instance, research from the Mayo Clinic indicates that abdominal obesity increases cardiovascular risk by promoting plaque buildup in arteries.
Another study underscores the psychological aspect: chronic stress and high cortisol can create a feedback loop with poor sleep and emotional eating, further driving fat accumulation. Interventions targeting stress reduction have shown promise in reducing visceral fat, suggesting that the mechanism is reversible with lifestyle changes.
To aid comprehension, a diagram comparing visceral vs. subcutaneous fat distribution—perhaps a cross-sectional body image with shaded areas—would illustrate why visceral fat is more dangerous and how cortisol targets it specifically.
Managing Cortisol Belly: Actionable Strategies
Now that we've explored the science, let's turn to what you can do. As someone who's navigated stress-related weight challenges myself, I know it's empowering to have practical steps. Remember, managing cortisol belly isn't about quick fixes but sustainable habits that address the root cause—chronic stress.
First, prioritize stress management techniques. Practices like mindfulness meditation or yoga can lower cortisol levels by calming the HPA axis. Aim for 10-15 minutes daily; consistency is key.
Second, focus on a balanced diet rich in anti-inflammatory foods. Reduce refined sugars and incorporate omega-3s from sources like salmon or walnuts, which help counteract cortisol's effects on insulin resistance. Pair this with regular exercise—mix cardio (like walking) with strength training to build muscle and boost metabolism.
Third, ensure quality sleep, as poor rest elevates cortisol. Target 7-9 hours per night and establish a wind-down routine.
For actionable takeaways:
- Track Your Stress: Keep a journal to identify triggers and monitor how they affect your eating habits.
- Incorporate Movement: Engage in 150 minutes of moderate exercise weekly, such as brisk walking, to reduce visceral fat.
- Seek Professional Help: If stress feels overwhelming, consult a healthcare provider for personalized advice, possibly including therapy.
By addressing these, you can break the cycle of cortisol-driven fat gain. At BeSlim.me, we've helped many reclaim their health this way, and I believe you can too.
In summary, cortisol belly stems from chronic stress disrupting hormonal balance and favoring visceral fat storage. With understanding and action, it's manageable. For deeper insights, Cleveland Clinic's overview on stress and weight gain provides additional evidence on these connections.
References
- Studies on chronic stress show elevated cortisol linked to increased visceral fat - ncbi.nlm.nih.gov
- Research from the Mayo Clinic indicates that abdominal obesity increases cardiovascular risk - mayoclinic.org
- Cleveland Clinic's overview on stress and weight gain - health.clevelandclinic.org
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.