As the Founder and Chief Scientific Officer of BeSlim.me, I've spent years guiding individuals through their weight loss journeys, and one pattern I've seen time and again is how chronic stress sabotages even the best intentions. You might be eating right and exercising, but if stress is a constant companion, that stubborn belly fat just won't budge. I understand how frustrating this can be—it's not just about willpower; it's about biology. In this deep dive, we'll explore the cortisol-insulin spiral and why stress literally gets stored as belly fat. My goal is to empower you with knowledge so you can take control. Let's dive into the science behind this.
Understanding Cortisol: The Stress Hormone's Role in the Body
Cortisol, often dubbed the "stress hormone," is produced by the adrenal glands in response to stressors, whether physical, emotional, or environmental. This hormone is essential for survival, orchestrating the body's fight-or-flight response by mobilizing energy reserves. However, when stress becomes chronic, cortisol levels remain elevated, leading to a cascade of metabolic disruptions.
At the cellular level, cortisol binds to glucocorticoid receptors found in nearly every tissue, influencing gene expression and metabolic pathways. It promotes gluconeogenesis in the liver, breaking down proteins and fats to produce glucose for immediate energy. This mechanism is adaptive in short bursts but problematic over time, as it can lead to insulin resistance and fat redistribution.
Chronic elevation of cortisol disrupts the hypothalamic-pituitary-adrenal (HPA) axis, the body's central stress response system. This dysregulation not only sustains high cortisol but also affects other hormones, setting the stage for weight gain. For instance, studies show that prolonged stress correlates with increased visceral fat accumulation, particularly around the abdomen.
To visualize this, a simple diagram illustrating the HPA axis feedback loop would be helpful here—showing the hypothalamus releasing corticotropin-releasing hormone (CRH), stimulating the pituitary to release adrenocorticotropic hormone (ACTH), and finally the adrenals producing cortisol, with arrows indicating negative feedback under normal conditions versus dysregulation in chronic stress.
The Cortisol-Insulin Connection: A Vicious Cycle
The interplay between cortisol and insulin forms a spiral that exacerbates fat storage. Insulin, produced by the pancreas, regulates blood sugar by facilitating glucose uptake into cells. Under normal circumstances, it promotes energy storage as glycogen or fat. However, elevated cortisol interferes with this process by inducing insulin resistance, where cells become less responsive to insulin's signals.
Mechanistically, cortisol activates enzymes like phosphoenolpyruvate carboxykinase (PEPCK) in the liver, enhancing glucose production while simultaneously inhibiting insulin's suppressive effects on gluconeogenesis. This leads to higher blood glucose levels, prompting the pancreas to release more insulin—a state known as hyperinsulinemia. Over time, this resistance means glucose isn't efficiently stored in muscles or liver, instead being converted to triglycerides and deposited as fat, especially in visceral areas.
Furthermore, cortisol stimulates appetite-regulating hormones like neuropeptide Y, increasing cravings for high-calorie foods, which further spikes insulin. This cycle is self-perpetuating: stress raises cortisol, which blunts insulin sensitivity, leading to more fat storage and potentially more stress from weight gain.
A comparison table could enhance understanding here, contrasting acute stress (short-term cortisol spike, adaptive energy mobilization) versus chronic stress (sustained cortisol, insulin resistance, visceral fat gain). Columns might include "Hormonal Response," "Metabolic Effect," and "Long-Term Outcome" for clarity.
Research supports this mechanism; for example, chronic stress linked to insulin resistance and abdominal obesity highlights how cortisol dysregulation contributes to metabolic syndrome.
Why Stress Targets Belly Fat: The Biology of Visceral Storage
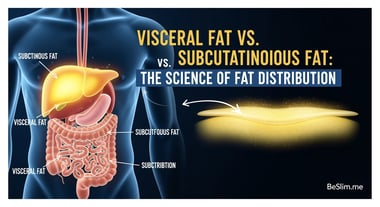
Belly fat, or visceral adipose tissue, is particularly susceptible to the cortisol-insulin spiral due to its unique biology. Unlike subcutaneous fat, visceral fat surrounds organs like the liver and intestines, and it's metabolically active, releasing free fatty acids directly into the portal vein, which affects liver function and systemic metabolism.
Cortisol promotes lipolysis in peripheral fats but encourages lipogenesis in abdominal areas through its action on 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1), an enzyme that converts inactive cortisone to active cortisol within fat cells. This local amplification of cortisol in visceral tissue enhances fat cell proliferation and lipid accumulation. Insulin, in this resistant state, fails to inhibit hormone-sensitive lipase effectively, allowing continued fat breakdown elsewhere while favoring storage in the abdomen.
Cell signaling pathways, such as the activation of peroxisome proliferator-activated receptor gamma (PPARγ), are upregulated by cortisol, promoting adipocyte differentiation specifically in visceral depots. This explains why stressed individuals often develop an "apple-shaped" body, with fat centralized around the midsection, increasing risks for conditions like type 2 diabetes and cardiovascular disease.
The preference for belly fat storage is also tied to evolutionary biology—quick energy access near vital organs during threats—but in modern chronic stress, it becomes maladaptive. Supporting this, elevated cortisol associated with visceral fat accumulation underscores the link to metabolic disorders.
Breaking the Spiral: Strategies to Reduce Cortisol and Shed Belly Fat
Now that we've unpacked the science, let's shift back to what this means for you. As someone who's helped countless people at BeSlim.me, I can tell you that breaking this cycle is possible with targeted, evidence-based strategies. The key is addressing stress at its root while supporting metabolic health—it's not just about dieting; it's about holistic balance.
Start by incorporating stress-reduction techniques like mindfulness meditation or yoga, which can lower cortisol levels by modulating the HPA axis. Aim for 10-15 minutes daily; consistency is crucial. Pair this with regular physical activity, such as moderate aerobic exercise, which enhances insulin sensitivity and promotes fat loss from visceral areas without spiking cortisol excessively.
Nutritionally, focus on a balanced diet rich in anti-inflammatory foods—think leafy greens, fatty fish, and nuts—to counteract cortisol's effects. Avoid high-sugar foods that exacerbate insulin spikes. For instance, intermittent fasting has shown promise in resetting insulin responses, but consult a professional to tailor it to your needs.
Sleep is non-negotiable; prioritize 7-9 hours per night, as poor sleep elevates cortisol. Track your progress with simple metrics like waist circumference or stress journals to stay motivated.
Here are some actionable takeaways to get started:
- Daily Stress Check-In: Spend 5 minutes journaling stressors and one positive action to address them—this builds resilience.
- Meal Planning Tip: Incorporate fiber-rich foods in every meal to stabilize blood sugar and reduce insulin surges.
- Exercise Routine: Try 30 minutes of walking or yoga three times a week to lower cortisol without overexertion.
- Professional Support: If stress feels overwhelming, seek guidance from a healthcare provider or coach like those at BeSlim.me.
Remember, you're not alone in this. By understanding and acting on the cortisol-insulin spiral, you can reclaim control over your body and health. Evidence from lifestyle interventions reducing cortisol and abdominal fat confirms that these changes can lead to measurable improvements.
References
- Chronic stress linked to insulin resistance and abdominal obesity - ncbi.nlm.nih.gov
- Elevated cortisol associated with visceral fat accumulation - mayoclinic.org
- Lifestyle interventions reducing cortisol and abdominal fat - cdc.gov
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.