Hello, I'm Master Kim, the founder and Chief Scientific Officer of BeSlim.me. I've spent years diving into the science of weight management, drawing from my own experiences with sleep struggles and how they've affected my appetite. If you've ever woken up after a rough night feeling ravenous, you're not alone—I've been there too. It's frustrating when poor sleep seems to sabotage your efforts to eat mindfully. In this article, we'll explore how sleep deprivation ramps up hunger through the ghrelin-leptin connection, and I'll share some insights to help you take control. Let's dive into the science behind this to understand why it happens and what you can do about it.
Understanding Ghrelin and Leptin: The Hunger Hormones
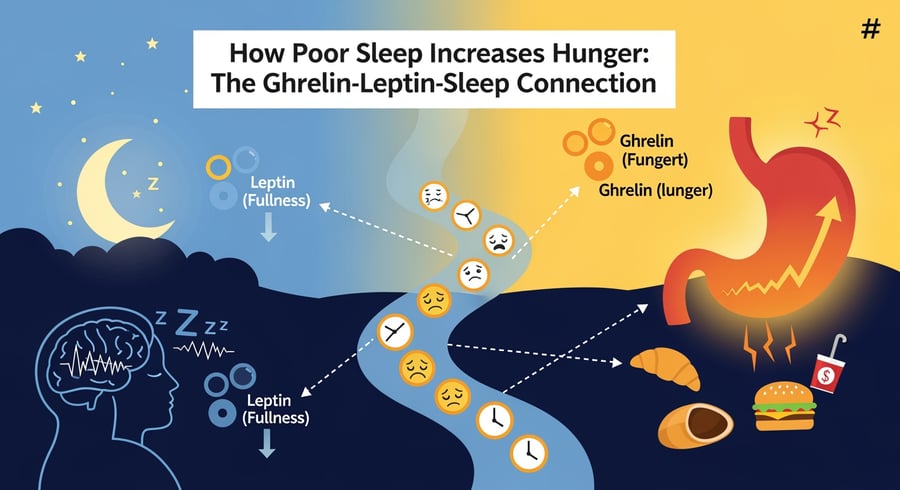
Ghrelin and leptin are key players in regulating appetite and energy balance in the body. Ghrelin, often called the "hunger hormone," is primarily produced in the stomach and signals the brain to increase appetite, prompting you to eat. It rises before meals and falls after eating, acting as a messenger that tells your body it's time to refuel. On the other hand, leptin is produced by fat cells and acts as a satiety signal, informing the brain when you've had enough food, which helps prevent overeating.
These hormones don't work in isolation; they interact with the body's overall metabolic system. Ghrelin stimulates the release of growth hormone from the pituitary gland and influences reward pathways in the brain, making food seem more appealing. Leptin, conversely, binds to receptors in the hypothalamus, a brain region that controls hunger and energy expenditure, to suppress appetite and increase metabolism.
When sleep is disrupted, this delicate balance shifts. Poor sleep can elevate ghrelin levels while suppressing leptin, creating a perfect storm for increased hunger. This isn't just about feeling tired—it's a hormonal imbalance that drives cravings, especially for high-calorie foods. To visualize this interplay, a simple comparison table could be helpful here: one column for ghrelin (role: stimulates hunger; production site: stomach; effect of poor sleep: increases) and another for leptin (role: suppresses hunger; production site: fat cells; effect of poor sleep: decreases). This table would make it easier to grasp how these hormones oppose each other and why sleep matters.
Let's transition to the research: Studies show that even short-term sleep restriction can alter these hormones significantly. For instance, sleep deprivation leads to increased ghrelin and decreased leptin levels, contributing to greater hunger and caloric intake.
The Impact of Sleep Deprivation on Ghrelin and Leptin Levels
Sleep deprivation disrupts the natural rhythms of ghrelin and leptin, leading to heightened hunger. During a normal sleep cycle, ghrelin levels typically decrease at night, allowing the body to rest without constant hunger signals. However, when sleep is cut short—say, to less than seven hours—ghrelin production ramps up. This increase can persist into the next day, making you feel hungrier than usual.
Leptin follows an opposite pattern: its levels naturally rise during sleep, promoting feelings of fullness. With inadequate sleep, leptin production drops, weakening the body's ability to signal satiety. The result? You're not only hungrier but also less satisfied after eating, which can lead to overconsumption. This effect is compounded by how sleep loss affects the brain's reward centers, making sugary or fatty foods more irresistible.
Research highlights the severity of these changes. In one study, participants who slept only four hours per night for two nights experienced a 28% increase in ghrelin and an 18% decrease in leptin compared to those who slept ten hours. This hormonal shift correlated with a 24% increase in hunger and a preference for calorie-dense foods. Such findings underscore why chronic sleep issues often link to weight gain.
For better understanding, a diagram illustrating the daily fluctuations of ghrelin and leptin in well-rested versus sleep-deprived individuals would be ideal. It could show ghrelin spiking higher and leptin dipping lower in the sleep-deprived curve, with arrows indicating brain signaling for hunger. This visual would clarify the temporal dynamics and emphasize sleep's role in hormonal regulation.
Diving deeper into the science, the mechanism involves the body's circadian rhythm, governed by the suprachiasmatic nucleus in the brain. Disrupted sleep misaligns this internal clock, affecting hormone secretion. According to evidence from controlled trials, short sleep duration is associated with elevated ghrelin and reduced leptin, which may contribute to obesity risk over time.
The Biological Mechanisms: How Sleep Influences Hormone Regulation
At the cellular level, the connection between sleep, ghrelin, and leptin involves intricate signaling pathways. Ghrelin is synthesized in the gastric mucosa, where specialized cells called X/A-like cells release it in response to fasting or energy needs. Sleep deprivation activates stress responses, such as elevated cortisol from the adrenal glands, which in turn stimulates these cells to produce more ghrelin. This process involves the hypothalamic-pituitary-adrenal (HPA) axis: poor sleep triggers corticotropin-releasing hormone (CRH) release, leading to adrenocorticotropic hormone (ACTH) and cortisol, which indirectly boosts ghrelin secretion.
On the leptin side, adipocytes (fat cells) produce leptin proportional to body fat stores. During sleep, particularly slow-wave sleep, the body enhances leptin release through sympathetic nervous system modulation. Sleep loss disrupts this by increasing sympathetic activity, which inhibits leptin production. At the molecular level, this involves gene expression: sleep deprivation downregulates the LEP gene in adipocytes, reducing leptin mRNA and subsequent protein synthesis.
These mechanisms converge in the hypothalamus, where ghrelin binds to growth hormone secretagogue receptors (GHS-R), activating orexigenic neurons that promote hunger. Leptin, binding to its receptors (Ob-R), activates anorexigenic neurons to curb appetite. Poor sleep tilts this balance toward orexigenic activity, enhancing hunger signals via neuropeptide Y and agouti-related peptide pathways while diminishing pro-opiomelanocortin signals that promote satiety.
Furthermore, sleep influences insulin sensitivity, which interacts with these hormones. Reduced sleep impairs glucose metabolism, leading to insulin resistance that can amplify ghrelin's effects and further suppress leptin. This creates a feedback loop where hunger drives eating, potentially worsening sleep through digestive discomfort or caffeine reliance.
To enhance comprehension, a flowchart diagram could depict this: starting with "Sleep Deprivation" leading to "HPA Axis Activation" → "Increased Cortisol" → "Elevated Ghrelin from Stomach Cells" and parallel paths for "Sympathetic Overactivity" → "Reduced Leptin from Adipocytes" → "Hypothalamic Imbalance" → "Increased Hunger." Such a visual would break down the complex cell signaling into digestible steps.
The scientific backing is clear: Investigations reveal that chronic sleep restriction alters ghrelin and leptin through neuroendocrine pathways, linking it to metabolic disorders like obesity and type 2 diabetes.
Actionable Takeaways: Improving Sleep to Balance Hunger Hormones
Now that we've explored the science, let's bring this back to you. As someone who's navigated these challenges personally, I know small changes can make a big difference. Prioritizing sleep isn't just about feeling rested—it's a powerful tool for managing hunger and supporting your weight goals at BeSlim.me.
Here are some practical steps based on the mechanisms we've discussed:
Aim for 7-9 Hours of Quality Sleep: Consistency helps regulate your circadian rhythm, stabilizing ghrelin and leptin. Establish a bedtime routine, like dimming lights an hour before bed, to signal your body it's time to wind down.
Manage Stress to Curb Cortisol Spikes: Since elevated cortisol from poor sleep boosts ghrelin, incorporate relaxation techniques such as meditation or deep breathing. Even 10 minutes daily can reduce HPA axis overactivity.
Time Your Meals Mindfully: Eat your last meal 2-3 hours before bed to avoid disrupting sleep and hormone balance. Focus on balanced nutrition to support leptin production—think lean proteins, healthy fats, and fiber-rich foods.
Monitor and Adjust: Track your sleep and hunger patterns using a journal or app. If you notice cravings after short nights, counteract with protein-packed snacks to help suppress ghrelin naturally.
Seek Professional Guidance if Needed: If sleep issues persist, consult a healthcare provider to rule out conditions like sleep apnea, which can exacerbate hormonal imbalances.
By addressing sleep, you're directly influencing the ghrelin-leptin axis, reducing unnecessary hunger and making it easier to maintain a healthy lifestyle. Remember, these changes compound over time—start small, and you'll likely see improvements in both your energy and appetite control. At BeSlim.me, we're here to support you on this journey.
References
- Sleep deprivation leads to increased ghrelin and decreased leptin levels - pubmed.ncbi.nlm.nih.gov
- Short sleep duration is associated with elevated ghrelin and reduced leptin - ncbi.nlm.nih.gov
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.