Hello, I'm Master Kim, the founder and Chief Scientific Officer of BeSlim.me. Drawing from my years of experience in health sciences and helping countless individuals achieve sustainable weight management, I've seen firsthand how misconceptions about body fat can hinder progress. You might think of fat as just stored energy or something to eliminate, but it's far more complex and vital. In this article, we'll explore adipose tissue—what it truly is and why it's a critical endocrine organ that influences your overall health. Whether you're aiming to understand your body better or seeking ways to optimize your wellness, I hope this empowers you. Let's dive into the science behind this.
What Is Adipose Tissue? Understanding the Basics
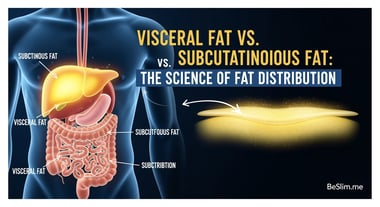
Adipose tissue, commonly known as body fat, is a specialized connective tissue composed primarily of adipocytes, which are cells designed to store energy in the form of lipids. Far from being inert, adipose tissue plays essential roles in energy homeostasis, insulation, and protection of vital organs. It exists throughout the body, from subcutaneous layers under the skin to visceral deposits around internal organs.
At its core, adipose tissue consists of two main types: white adipose tissue (WAT) and brown adipose tissue (BAT). White adipose tissue is the predominant form in adults, responsible for storing excess energy as triglycerides. In contrast, brown adipose tissue is more metabolically active, generating heat through a process called thermogenesis. There's also beige adipose tissue, which can emerge from white fat under certain conditions like cold exposure, exhibiting properties similar to brown fat.
To visualize this, a simple comparison table could enhance understanding here:
| Type of Adipose Tissue | Primary Function | Location in Body | Key Characteristics |
|---|---|---|---|
| White (WAT) | Energy storage | Subcutaneous and visceral | Large lipid droplets, fewer mitochondria |
| Brown (BAT) | Heat production | Neck, upper back | High mitochondrial content, rich in blood vessels |
| Beige | Adaptive thermogenesis | Within white fat depots | Can "brown" in response to stimuli like exercise |
This table highlights the diversity within adipose tissue, showing it's not a monolithic entity but a dynamic system. Biologically, adipocytes originate from mesenchymal stem cells through a process called adipogenesis, regulated by transcription factors such as PPARγ (peroxisome proliferator-activated receptor gamma). This differentiation involves cell signaling pathways where hormones like insulin promote lipid accumulation, while others like glucagon trigger breakdown.
Adipose tissue also interacts with the nervous system via sympathetic innervation, which can stimulate lipolysis—the release of fatty acids into the bloodstream for energy use. This mechanism underscores why adipose tissue is integral to metabolic balance, adapting to nutritional status and environmental cues.
The Structure and Composition of Adipose Tissue
Delving deeper, the structure of adipose tissue reveals a complex matrix beyond just fat cells. Adipocytes make up about 80-90% of the tissue's volume but only 10-20% of its cell population. The remaining cells include preadipocytes, fibroblasts, immune cells like macrophages, and endothelial cells forming blood vessels. This stromal vascular fraction supports the tissue's functionality, enabling nutrient exchange and inflammatory responses.
In white adipose tissue, each adipocyte contains a large, single lipid droplet that occupies most of the cell's volume, pushing the nucleus to the periphery. The cell membrane is equipped with receptors for hormones such as insulin, which activates the PI3K-Akt pathway to facilitate glucose uptake and triglyceride synthesis. Conversely, catecholamines bind to beta-adrenergic receptors, initiating a cascade via cAMP that activates hormone-sensitive lipase, breaking down triglycerides into glycerol and free fatty acids.
Brown adipose tissue, however, features multiple small lipid droplets and abundant mitochondria rich in uncoupling protein 1 (UCP1). This protein allows protons to leak across the mitochondrial membrane, dissipating energy as heat rather than ATP production—a key mechanism in non-shivering thermogenesis. The signaling here involves noradrenaline from sympathetic nerves, activating adenylyl cyclase to increase cAMP levels, which then upregulates UCP1 expression.
A diagram illustrating the cellular structure of WAT versus BAT would be particularly helpful at this point. For instance, it could show the unilocular (single droplet) nature of white adipocytes contrasted with the multilocular (multiple droplets) brown ones, complete with labeled mitochondria and signaling pathways. Such a visual aid would clarify how structural differences translate to functional disparities.
Moreover, adipose tissue's extracellular matrix, composed of collagen and other proteins, provides structural integrity and facilitates cell-to-cell communication. Dysregulation in this matrix, often seen in obesity, can lead to fibrosis and impaired tissue function, highlighting the tissue's responsiveness to physiological changes.
According to research, adipose tissue composition varies by location and influences metabolic health, with visceral fat being more prone to inflammation due to its proximity to organs and higher macrophage infiltration.
Adipose Tissue as an Endocrine Organ: Hormones and Signaling
Transitioning to its endocrine role, adipose tissue functions as a dynamic organ that secretes over 600 bioactive molecules, collectively known as adipokines. These include hormones like leptin and adiponectin, which regulate appetite, insulin sensitivity, and inflammation systemically.
Leptin, produced primarily by white adipocytes, acts on the hypothalamus via the JAK-STAT signaling pathway to suppress appetite and increase energy expenditure. Its levels correlate with fat mass, providing a feedback loop to maintain energy balance. In obesity, however, leptin resistance can occur, where high circulating levels fail to signal satiety, exacerbating weight gain.
Adiponectin, conversely, enhances insulin sensitivity by activating AMPK (AMP-activated protein kinase) in muscle and liver tissues, promoting fatty acid oxidation and glucose utilization. Low adiponectin levels are associated with metabolic disorders, underscoring adipose tissue's influence on whole-body metabolism.
Other adipokines, such as resistin and visfatin, modulate inflammation and insulin resistance. For instance, in inflamed adipose tissue, macrophages release pro-inflammatory cytokines like TNF-α, which activate NF-κB pathways, leading to insulin resistance through serine phosphorylation of IRS-1 (insulin receptor substrate-1).
Brown adipose tissue contributes endocrinologically too, secreting factors like irisin, which can induce browning of white fat, enhancing thermogenic capacity. This process involves PGC-1α (peroxisome proliferator-activated receptor gamma coactivator 1-alpha), a transcriptional coactivator that boosts mitochondrial biogenesis.
The endocrine function extends to cross-talk with other organs: adipose-derived factors influence bone remodeling, cardiovascular health, and even brain function. For example, adipokines from adipose tissue play a role in regulating energy homeostasis and inflammation, linking fat mass to systemic diseases.
A flowchart diagram depicting the signaling pathways of key adipokines—from secretion in adipocytes to target organs—would greatly enhance comprehension here, illustrating feedback loops and interactions.
Health Implications and Why It Matters for You
The recognition of adipose tissue as an endocrine organ has profound implications for health. Excessive accumulation, particularly visceral fat, leads to chronic low-grade inflammation, contributing to conditions like type 2 diabetes and cardiovascular disease through disrupted adipokine balance.
Conversely, healthy adipose function supports metabolic flexibility—the ability to switch between fuel sources efficiently. Brown fat activation, for instance, can improve glucose tolerance and reduce obesity risk.
From a mechanistic viewpoint, interventions like exercise stimulate AMPK activation in adipocytes, promoting lipolysis and adipokine secretion favorable for insulin sensitivity. Caloric restriction can remodel adipose tissue, reducing inflammation via decreased macrophage infiltration and altered gene expression.
Research indicates that dysfunctional adipose tissue contributes to metabolic syndrome, emphasizing the need for targeted lifestyle approaches.
As we wrap up, let's consider some actionable takeaways. I recommend incorporating regular physical activity, such as 30 minutes of moderate exercise daily, to enhance brown fat activity and improve adipokine profiles. Focus on a balanced diet rich in anti-inflammatory foods like omega-3s to support healthy adipose function. If you're struggling with weight, tracking your body's signals—hunger cues influenced by leptin—can guide sustainable changes. At BeSlim.me, we've helped many by emphasizing these science-backed strategies, and I encourage you to consult a healthcare professional for personalized advice. Remember, understanding adipose tissue empowers you to view body fat not as an enemy, but as a vital partner in your health journey.
References
Medical Disclaimer
The content on this website is for informational and educational purposes only. It is not intended as medical advice and should not be relied upon as a substitute for consultations with qualified healthcare professionals who are familiar with your individual medical needs. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.